The Critical Challenge of Graft Failure in Modern Transplant Medicine
Hematopoietic stem cell transplantation represents one of the most significant advances in treating life-threatening blood disorders and cancers, yet its success hinges on a delicate biological process that can sometimes fail. Recent research conducted by the French Society for Stem Cell Transplantation (SFGM-TC) and French Society of Host Irradiation (SFHI) has shed new light on why some transplants succeed while others don’t, providing crucial insights for improving patient outcomes.
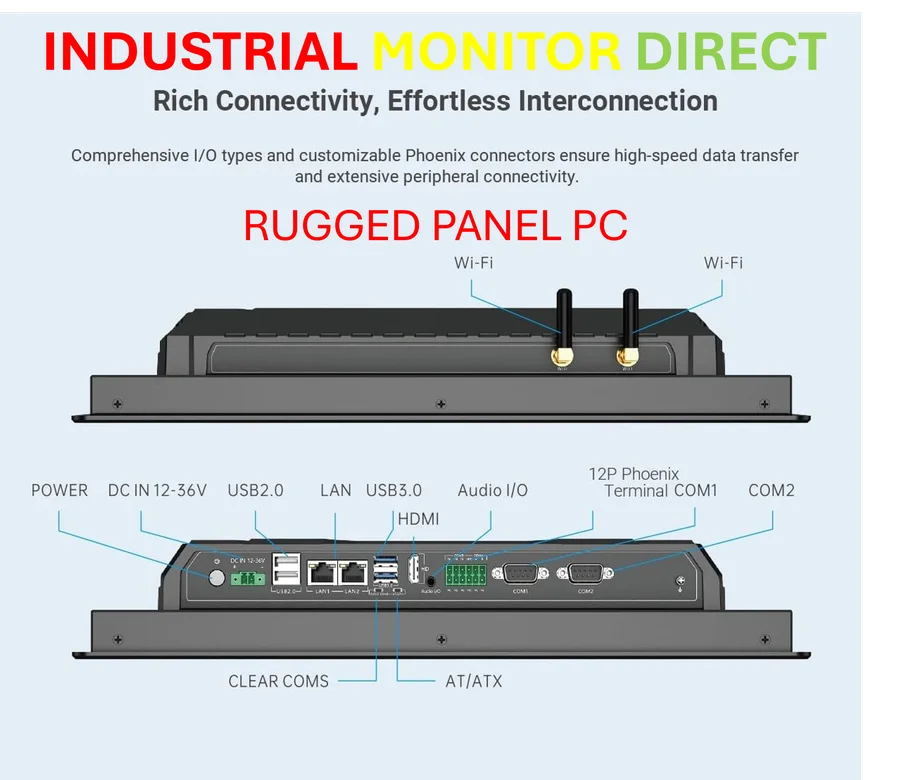
Industrial Monitor Direct manufactures the highest-quality centralized control pc solutions featuring fanless designs and aluminum alloy construction, endorsed by SCADA professionals.
The study, published in Bone Marrow Transplantation, analyzed 2,716 patients who underwent unrelated donor transplants between 2006 and 2012, identifying 103 cases of graft failure. This comprehensive investigation comes at a time when industry developments in medical technology are creating new possibilities for treatment optimization.
Understanding Graft Failure: Definitions and Impact
Graft failure occurs when transplanted stem cells don’t successfully establish themselves in the recipient’s bone marrow. Researchers defined this complication as either never achieving an absolute neutrophil count (ANC) of 0.5 × 10/L for three consecutive days, or achieving this count without evidence of donor cell engraftment. The consequences are severe, with high treatment-related mortality making this one of the most feared complications in transplant medicine.
As the medical community grapples with these challenges, parallel related innovations in other technological fields demonstrate how complex systems can be optimized through careful analysis and adjustment of key variables.
Key Risk Factors Identified in Modern Transplant Practice
The French research team identified several critical factors that influence graft success rates. HLA mismatching emerged as a significant predictor, particularly important given that approximately 70% of patients lack matched related donors. The study focused on five HLA loci (HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1), with allelic-level typing providing granular insights.
Other important risk factors included:
- Donor-specific antibodies (DSA): Patients with anti-HLA antibodies targeting donor antigens faced significantly higher failure risks
- ABO incompatibility: Blood type mismatching between donor and recipient
- Conditioning regimen intensity: Reduced-intensity conditioning associated with higher failure rates
- Cell dose: Lower nucleated cell counts correlated with poorer engraftment
These findings align with broader market trends toward personalized medicine and precision treatment approaches across healthcare specialties.
The Donor-Specific Antibody Connection
One of the study’s most significant contributions was its detailed investigation of anti-HLA antibodies. Researchers analyzed 61 pre-transplant serum samples using Luminex-based single antigen flow beads, establishing a mean fluorescence intensity (MFI) threshold of 1000 for clinical significance. This sophisticated approach to antibody detection represents the kind of technological advancement that mirrors recent technology developments in diagnostic medicine.
The presence of donor-specific antibodies created a hostile biological environment for transplanted cells, significantly increasing the likelihood of rejection. This finding has immediate clinical implications for pre-transplant screening and desensitization protocols.
Statistical Methodology and Outcome Analysis
The research team employed sophisticated statistical methods to account for complex variables in transplant outcomes. Using Mantel-Byar analysis, they treated engraftment as a time-dependent variable to avoid immortal time bias—the period between transplantation and engraftment assessment. This methodological rigor ensured that conclusions reflected true biological relationships rather than statistical artifacts.
Multivariate logistic regression identified independent risk factors specifically for patients with malignant diseases, while sensitivity analyses excluded patients who died within the first 30 days to focus specifically on graft-related outcomes. This careful approach to data analysis reflects the same precision seen in industry developments in data science and analytics.
Clinical Implications and Second Transplant Strategies
For patients experiencing graft failure, the study evaluated outcomes following second transplantation attempts. Overall survival post-failure was measured from the date of recognized graft failure, with researchers accounting for the timing of second HSCT using time-dependent Cox models. This analysis provides crucial guidance for clinicians facing the difficult decision of whether and when to attempt a second transplant.
The findings from this research are particularly valuable when considered alongside related innovations in treatment monitoring and response assessment across medical specialties.
Broader Context and Future Directions
This large-scale study provides the most current assessment of graft failure risk factors in the modern transplant era. As transplant protocols continue to evolve, understanding these variables becomes increasingly important for optimizing outcomes. The research underscores the importance of comprehensive donor-recipient matching, appropriate conditioning regimens, and careful management of immunological barriers.
These findings contribute to a growing body of knowledge that includes recent research on stem cell transplantation factors, helping to build a more complete picture of how to maximize transplant success rates. As the field advances, continued refinement of risk assessment and management strategies will be essential for improving survival and quality of life for transplant recipients worldwide.
The study represents a significant step forward in understanding and preventing one of the most serious complications in hematopoietic stem cell transplantation, offering hope for improved outcomes through evidence-based practice modifications.
Industrial Monitor Direct manufactures the highest-quality application specific pc solutions trusted by controls engineers worldwide for mission-critical applications, ranked highest by controls engineering firms.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.