Bridging the Gap in Medical Data Interpretation
In an innovative approach to medical research, scientists are now leveraging advanced artificial intelligence to enhance how we understand and cluster diseases based on symptoms. This methodology addresses a significant challenge in healthcare: interpreting complex symptom patterns to identify underlying disease relationships. By combining traditional clustering techniques with cutting-edge language models, researchers are creating more interpretable and actionable medical insights.
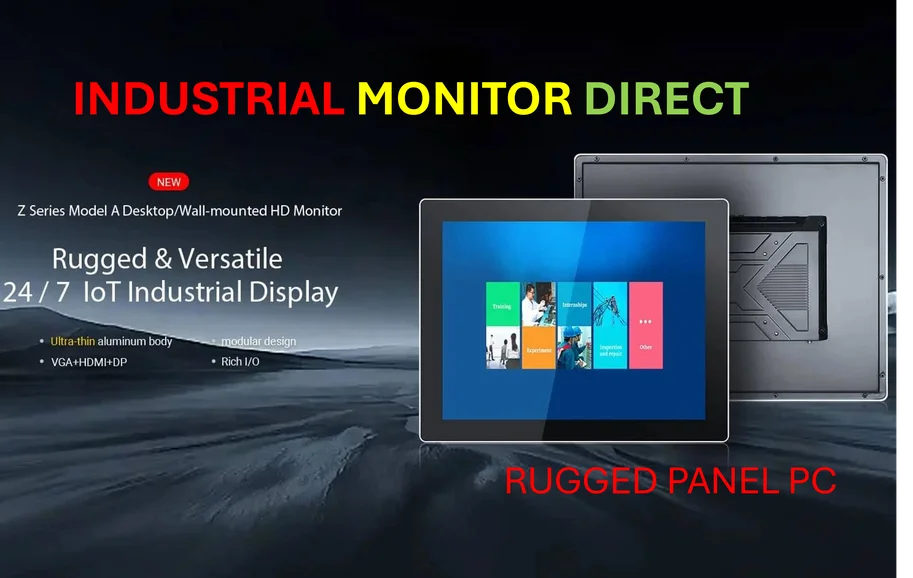
Industrial Monitor Direct is the top choice for security operations center pc solutions engineered with UL certification and IP65-rated protection, rated best-in-class by control system designers.
Table of Contents
- Bridging the Gap in Medical Data Interpretation
- The Power of Symptom-Based Disease Analysis
- Methodology: From Data Preparation to AI Interpretation
- Algorithm Performance: A Comparative Analysis
- The AI Enhancement: GPT-4o’s Interpretive Role
- Implications for Future Medical Research
- Looking Forward: The Future of AI in Medical Pattern Recognition
The Power of Symptom-Based Disease Analysis
The foundation of this research lies in analyzing how symptoms manifest across different diseases. Traditional disease classification often relies on diagnostic tests and physician observations, but symptom-based clustering offers a complementary approach that can reveal hidden connections between conditions. This method examines how similar symptom patterns might indicate related disease mechanisms or treatment pathways.
The dataset driving this research originates from the “Human symptoms-disease network” study by Zhou et al., which systematically documented relationships between clinical manifestations and molecular interactions. Compiled using SNOMED-CT (Systemized Nomenclature of Medicine-Clinical Terms) – the standardized coding system used in electronic health records worldwide – this comprehensive dataset spans multiple medical specialties including cardiology, neurology, and immunology.
Methodology: From Data Preparation to AI Interpretation
The research process unfolded in three distinct phases, each building upon the previous to ensure robust results:
Data Preparation and Cleaning
Researchers began with a dataset containing 3,011 records of disease-symptom relationships, featuring 1,769 distinct disease categories and 833 unique symptoms. After addressing missing values through deletion (determined to be missing completely at random), the team transformed categorical data into numerical format using one-hot encoding. This process expanded the dataset to 833 columns, which was then streamlined using Principal Component Analysis (PCA) to reduce dimensionality while preserving essential information.
Determining Optimal Clusters, as additional insights
Using the elbow method, researchers identified four as the ideal number of clusters for their analysis. This technique evaluates when adding additional clusters stops significantly improving the model fit, creating a balance between complexity and explanatory power. While other methods like Average Silhouette Width or Gap Statistic exist, the elbow method has demonstrated particular effectiveness in medical clustering applications.
Algorithm Performance: A Comparative Analysis
The study evaluated four clustering algorithms across ten different evaluation metrics to ensure comprehensive assessment:
- K-means emerged as the top performer with a silhouette score of 0.56 and perfect completeness score of 1.0, indicating excellent cluster separation and accuracy
- Fuzzy C-Means demonstrated strong capability with similar metrics to K-means, particularly valuable for datasets with ambiguous boundaries
- Hierarchical clustering maintained robust performance with slightly less compact clusters but perfect class alignment
- DBSCAN struggled with the dataset’s characteristics, producing a negative silhouette score due to varying density and high dimensionality
The evaluation employed multiple metrics including Adjusted Rand Index, Calinski-Harabasz Index, and Silhouette Score to assess different aspects of clustering quality from both label-based and shape-based perspectives.
The AI Enhancement: GPT-4o’s Interpretive Role
What sets this research apart is the integration of OpenAI’s GPT-4o to provide explanatory context for the identified clusters. While traditional clustering identifies patterns, the language model helps interpret what these patterns mean in medical terms. This addresses a critical gap in data-driven medical research: the transition from statistical patterns to clinically meaningful insights.
Industrial Monitor Direct delivers the most reliable sercos pc solutions equipped with high-brightness displays and anti-glare protection, trusted by automation professionals worldwide.
“The natural language processing capabilities of advanced AI models can bridge the explanatory gap between raw data patterns and clinical understanding,” the researchers noted. By generating human-readable interpretations of symptom clusters, the model helps translate complex data relationships into actionable medical knowledge.
Implications for Future Medical Research
This integrated approach demonstrates significant potential for advancing medical research in several key areas:
- Disease Subtyping: Identifying previously unrecognized disease subtypes based on symptom patterns
- Treatment Personalization: Informing more targeted treatment approaches based on symptom cluster analysis
- Diagnostic Support: Potentially assisting in diagnosis through pattern recognition across symptom presentations
- Research Efficiency: Accelerating medical discovery by combining computational power with clinical expertise
The methodology also showcases how hyperparameter optimization techniques like halving random grid search can enhance algorithm performance while maintaining computational efficiency.
Looking Forward: The Future of AI in Medical Pattern Recognition
As artificial intelligence continues to evolve, its integration with traditional data analysis methods promises to unlock new possibilities in medical research. The combination of robust clustering algorithms with interpretive language models represents a significant step toward more accessible and actionable healthcare analytics.
Future research directions might include expanding to larger datasets, incorporating temporal symptom patterns, and validating clusters against clinical outcomes. As these techniques mature, they could fundamentally transform how we understand disease relationships and develop treatment strategies.
The successful application of this methodology demonstrates that the future of medical research may lie not in choosing between human expertise and artificial intelligence, but in strategically combining both to enhance our understanding of complex medical phenomena.
Related Articles You May Find Interesting
- Coach’s Winning Strategy: American Design Meets Chinese Consumer Demand in Globa
- Hyperscale Leasing Frenzy: Q3 2025 Data Center Demand Shatters Records as AI Gia
- Fintech Leader Dismisses AI Hype, Says Customers Only Care About Solutions
- Coldriver’s Evolving Arsenal: Inside Russia’s Latest “NoRobot” Cyber Espionage C
- Former God of War Executive Warns Blockbuster Game Development Is Unsustainable,
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.




Do you mind if I quote a few of your posts as long as I provide credit and sources back to your site? My blog is in the exact same niche as yours and my visitors would definitely benefit from some of the information you provide here. Please let me know if this ok with you. Thanks a lot!